Police have launched an investigation into Castle Hill Hospital near Hull following a series of patient deaths linked to heart valve operations. Documents obtained by the BBC reveal that several patients suffered avoidable harm during Transcatheter Aortic Valve Implant (TAVI) procedures, with critical complications allegedly omitted from official death certificates.
Humberside Police confirmed the inquiry is in its early stages and no arrests have been made. The investigation follows growing concerns over the hospital’s TAVI programme, which at one point had a mortality rate three times higher than the UK average.
Families Unaware of Surgical Errors and Concealed Death Causes
One high-profile case involves Dorothy Readhead, an 87-year-old patient who died after her TAVI procedure went catastrophically wrong. Despite warnings that access via her right artery was unsafe, surgeons proceeded with the operation using the right side. Mrs Readhead lost five litres of blood, remained conscious for six hours, and died a week later. Her death certificate did not mention the operation, instead listing pneumonia and heart disease.
A 2021 Royal College of Physicians (RCP) review rated her care as “poor” and cited a “have a go” approach by the TAVI team. A follow-up review in 2024 concluded that the vascular injury caused during the procedure directly led to her death. Her family only learned the full details after being contacted by the BBC.
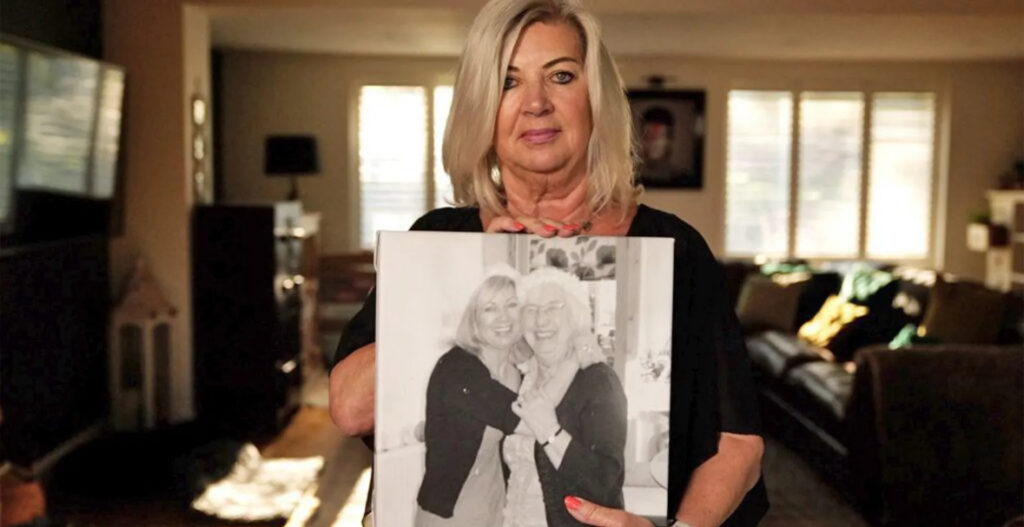
Another patient, Brian Hunter, died during his TAVI in 2021 after errors in deploying the device allowed blood to leak back into the heart. His family also received misleading information and were told he died from a heart attack. A later review graded his care as “very poor.”
Internal Warnings Ignored, Reviews Withheld from Families
Concerns about Castle Hill’s TAVI programme were flagged internally by seven cardiac consultants in 2021, who warned the hospital’s leadership about safety and transparency failures. They were alarmed that coroners were not informed of serious complications and that patient death causes were inaccurately recorded.
Three separate reviews—two by the RCP and one by external consultants IQ4U—have criticised poor clinical decision-making and inadequate documentation. None of the families were informed of these investigations until approached by the media.
Hospital Trust Defends Service Despite Reviews
The Humber Health Care Partnership, which operates Castle Hill through Hull University Teaching Hospitals NHS Trust, acknowledged past issues but said improvements have been made based on recommendations from the reviews. It maintains that the TAVI service remains essential and mortality rates have since stabilised.
However, the trust’s own data reportedly shows the unit’s mortality rate remains above the national average, despite its claim that three external reviews confirm it is now in line with national performance.
Calls for Accountability Amid Allegations of Concealment
The case has also highlighted wider concerns about NHS transparency and accountability. Former clinical director Dr Thanjavur Bragadeesh, who initially raised red flags about the TAVI programme, was later removed from his leadership role and eventually left the trust. He believes the findings of the 2024 RCP report validate his concerns.
Families of the deceased have expressed deep anger and distress. “To find out three years later what really happened is torturous,” said Tracy Fisher, daughter of Brian Hunter. “We feel like we were lied to — and that’s unforgivable.”
The police inquiry is expected to examine potential breaches in medical ethics, professional conduct, and the legal duty of candour, particularly in relation to how deaths were documented and communicated.