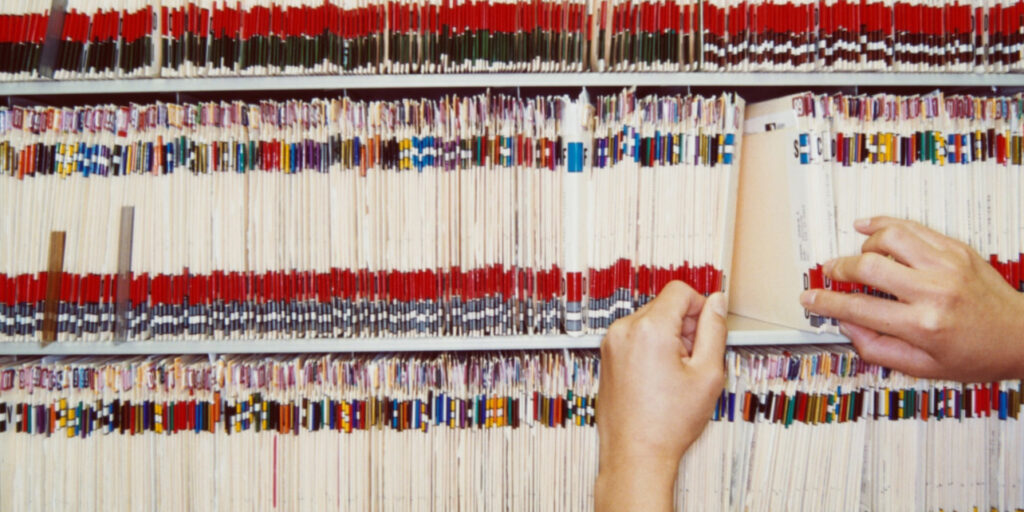
A major survey has revealed that nearly one in four patients in England have found mistakes in their NHS medical records, ranging from incorrect diagnoses to inaccurate medication details.
The findings raise fresh concerns about patient safety and the overall reliability of the health system’s record-keeping.
According to research conducted by Healthwatch England, 23% of adults surveyed said they had discovered errors or missing information in their personal health records.
These included incorrect names or dates of birth, inaccurate notes on past illnesses, or wrong details about medication and treatment.
Such mistakes have had serious consequences, with some patients being denied essential care, receiving incorrect medication, or missing out on necessary diagnostic tests.
In more severe cases, individuals were wrongly recorded as having illnesses they had never had or as having taken medication they had never been prescribed.
The survey, which included 1,800 adults across England, identified several types of errors:
– 26% were linked to personal details, such as name or date of birth
– 16% involved incorrect medication records
– 9% wrongly listed illnesses the patient had never experienced
– 9% falsely recorded medications given to treat specific ailments
Of those affected, 10% said they had been prescribed the wrong or inappropriate medication, while 12% said the errors led to being refused treatment. Others said the mistakes resulted in unsafe care or long delays in receiving the correct diagnosis.
The impact on patients goes beyond physical health. Many described the frustration and stress of constantly correcting their records or having to explain their medical history repeatedly. Healthwatch noted that correcting these issues is often time-consuming and places further pressure on patients and families.
Charities supporting patient care, including the Patients Association and National Voices, warned that such errors not only affect treatment but also undermine trust in the health service.
Mistakes are frequently traced to administrative oversights at GP surgeries or hospitals, often driven by strained resources, outdated IT systems, and fragmented communication across departments.
GP leaders and healthcare experts acknowledge that workforce shortages, high patient demand, and increasing bureaucracy contribute to these mistakes. There is growing concern that unless record-keeping improves, the risks to patient safety and quality of care will continue to rise.
The Department of Health and Social Care has responded by pledging to modernise NHS systems. As part of its wider digital transformation plan, it aims to introduce a unified patient record, accessible through the NHS app.
This will consolidate key health information such as diagnoses, test results, and referrals into a single digital record, designed to give patients better control over their own healthcare.
Despite these plans, campaigners and patients continue to call for urgent action to ensure the accuracy of medical records and to prevent further avoidable harm within the NHS.